
CT scan/MRI scan: eg, nodal distribution, staging of lymphoma.Ultrasonography may be helpful in evaluating the extent of lymph node involvement in patients with lymphadenopathy and may be more sensitive than CT scanning in some instances.CXR: sarcoidosis, TB, primary or secondary malignancy.Autoantibody screen: SLE, rheumatoid arthritis.Investigations for tuberculosis, syphilis serology, toxoplasma screen.Viral titres - eg, Epstein-Barr virus, HIV, hepatitis.Infection swabs from primary infection site for culture and sensitivities.įurther investigations will depend on the individual presentation but may include:.Investigation of patients with unexplained lymphadenopathy should include FBC, blood film and ESR, plasma viscosity or CRP (according to local policy).Investigations may not be required in cases of obvious cause and quick resolution with or without treatment. These will be governed by the history and examination and likely cause of lymphadenopathy. Roseola infantum - human herpesvirus type 6 (HHV-6).

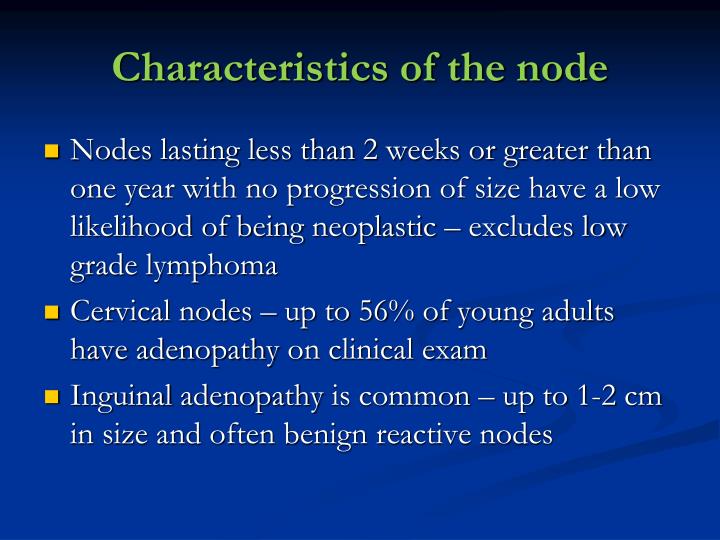
Perform a systematic examination to exclude signs of obvious malignancy and especially the abdomen to exclude hepatomegaly or splenomegaly. Measure body temperature to exclude pyrexia and check for any local sources of infection, including the scalp, skin, ears, nose, pharynx and chest. These are most prominent in the anterior cervical, inguinal and axillary regions and continue to increase in size until the age of 8-12, after which atrophy occurs. Most children have palpable lymph nodes, the relative size of which could qualify for lymphadenopathy in an adult. In adolescents a sexual history and history of intravenous drug use should be elicited. Presenting symptoms of more indolent diseases (eg, tuberculosis, malignancy) may occur some time after the development of the initial lymphadenopathy. īearing in mind the extensive list of differential diagnoses, it is important to keep the patient under review if spontaneous recovery does not occur. Supraclavicular and infraclavicular lymph nodes are always suspicious of an underlying malignancy, particularly in those aged over 40 years.

Persistent fever, night sweats, general malaise or weight loss may be pointers to significant disease. A history should include the duration of the lymphadenopathy, whether any other household members are acutely ill and whether there are any accompanying symptoms.


 0 kommentar(er)
0 kommentar(er)
